The outgoing Biden administration recently proposed a new rule to expand Medicare and Medicaid coverage. This rule, published on November 26, 2024, would finally allow for Medicare and Medicaid to treat obesity using anti-obesity medications. As of the time I am writing this, only 13 state Medicaid programs cover the cost of medications used to treat obesity. Medicare, due to wording in the 2006 Part D legislation, cannot do so at all. If this rule is passed, it will be an immense public health victory. Powerful new tools to treat obesity will be accessible to millions more people and this will quite literally save lives.
However, this rule is controversial. In this post, I am not going to go into the heated pricing debates about the drugs, the roles of insurance companies, the roles of pharmacy-benefits managers, or the other strings in our nation’s dysfunctional healthcare web. These are all important parts of the larger obesity medicine discussion. Above all of this, we–physicians, policy makers, politicians, insurance companies–must understand and internalize one extremely important scientific fact:
Obesity is a disease.
Obesity meets the accepted criteria for a disease
In medical science, we tend to follow the definition of a disease as clarified by organizations like the WHO:
“deviations from the normal or healthy structure or function of a part, organ, or system of the body, caused by underlying etiologies, manifested by characteristic symptoms and signs, and resulting in pathologic consequences that affect health, feeling, or functioning”
What does this mean in everyday speech? Essentially a disease needs to have four features:
- It is a change from the normal or healthy structure or function in the body
- It can be linked to an underlying cause or causes
- It has characteristic signs and symptoms
- It adversely affects a person’s health
How does obesity meet these criteria:
- There are accepted and well-researched parameters for body size and composition. In obesity, a person’s size and/or composition is significantly outside these norms.
- Obesity is the result of numerous complicated processes in the body that cause too much fat tissue to be deposited.
- Obesity has characteristic findings including abnormal measurements, but also abnormalities in things such as blood pressure, lab values, and increased risks of other diseases.
- Obesity affects health by leading to other diseases, by causing emotional distress due to severe weight bias in our society, and causing impairments in a person’s ability to move around.
Appetite
So what goes wrong with obesity? That is a very complicated question. In my opinion, weight regulation is one of the most complicated things that your body does. Other important body processes are well understood and somewhat straightforward. For example, we know to the molecular level what changes happen to make your heart conduct electrical signals or your muscles to contract. Weight regulation encompasses many different processes–from when and what you eat to how your body processes food.
The first part of this puzzle is appetite. This is how your body tells you to eat–how much, what you eat, when you eat, all of that. There are two major, competing pathways in your brain that regulate appetite: the hedonic or reward pathway, and the homeostatic pathway which I like to call the gut-brain pathway when explaining it.
Competing Pathways
The reward pathway is the pathway that is at play when you have cravings, when you stress eat, when you see something yummy or smell something delicious. It is a very powerful pathway, which is why it is so hard to resist cravings. This same pathway is what can lead to addictions in people. It can easily override the gut-brain pathway. It is also strongly linked with emotions and disturbances in emotions can lead to appetite issues.
The gut-brain pathway is the signalling from the rest of your body, including your stomach, to your brain. It gets signals when your stomach is full or empty and when your sugar levels are changing. Ideally, this would mean that you would only eat if your body needed fuel and you would stop eating as soon as your body was fueled.
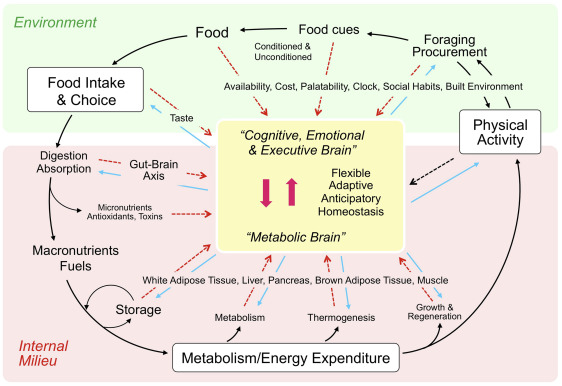
Berthoud, Hans-Rudolf et al. Gastroenterology, Volume 152, Issue 7, 1728 – 1738
Both pathways can be affected by emotions, other diseases, other medications, and the type of food you eat. For example, highly processed foods make your reward pathway overactive. Some people have stomachs that empty quicker than others so their brains get more “I’m hungry!” signals. Some other people have breakdowns in the signalling pathway so their brains never process “I’m full!” signals. Finally, some mental health conditions–such as ADHD or autism–can increase the reward pathway.
Hunger is a basic physical sensation
We know that appetite signalling is complicated. We also know that many things can affect it. Regardless of why you feel hungry, though, it’s important to remember that hunger is not a bad sensation. Hunger is an important and fundamental part of having a physical body, like feeling pain or the urge to go to the bathroom. Hunger is one of the first sensations we ever experience in life, and eating is our first big job as a newborn baby. There is a reason that starving to death is considered a particularly brutal way to die. Given all of this, it is not appropriate, compassionate, nor effective to expect people to just ignore intense hunger.
It also means that almost all of our hunger signals and appetite regulation is beyond our control. When your brain is telling you that you’re always hungry or that you only need to eat highly processed and calorie-dense food, it is not operating efficiently. This is one of the first things to understand about why obesity is a disease and not a moral or willpower failing.
The Centers for Medicare and Medicaid Services are accepting public comments on the proposed rule. They need to hear from Americans about how important this rule will be for our health! You can find more information about the proposed rule and tips for submitting a comment at the Obesity Action Coalition’s website, found here.
Very informative and useful information I am a rewards eater triggered by boredom and stress